Vocal-fold cyst
Vocal fold cysts are benign masses of the membranous vocal folds.[1] These cysts are enclosed, sac-like structures that are typically of a yellow or white colour.[2] They usually form unilaterally on the midpoint of the medial edge of the vocal folds.[1] However, they can form on the cephalic, or upper/superior, surface of the vocal folds as well.[1] There are two types of vocal fold cysts that differ in terms of location:[1]
- Sub-epithelial vocal fold cysts which are located in the superficial lamina propria of the vocal folds.[1]
- Ligament vocal fold cysts which are located within the deeper layers of the lamina propria or on the vocal ligament.[1]
The symptoms of vocal fold cysts vary but commonly include a hoarse voice and problems with the pitch of the voice. Initial treatment of the cysts involves voice therapy to reduce harmful vocal behaviours. If symptoms remain, patients may require surgery to remove the cyst. Surgery is typically followed by vocal rest and further voice therapy to restore voice function. Cysts may also be treated using vocal fold steroid injection.
Causes
There are several causes of vocal fold cysts:
- They can be congenital.[1]
- They can result from the blockage of a mucous gland's excretory duct.[3] In this case, they are sometimes referred to as retention cysts.[3]
- They can be the result of phonotrauma.[1] Phonotrauma refers to behaviours that can lead to vocal fold injuries, such as vocal overuse (i.e. too much speaking), vocal misuse (i.e. speaking in an unnaturally high or low pitch), or vocal abuse (i.e. yelling or whispering for prolonged periods).[4] Vocal folds vibrate during phonation resulting in repeated collisions of the right and left vocal folds.[4] Phonotrauma subjects the vocal folds to excessive mechanical forces during these vibratory cycles, which can lead to the development of a wound.[4] It is the healing of these wounds, which leads to tissue re-structuring, that can result in a vocal fold cyst.[4]
Signs and Symptoms
Both sub-epithelial vocal fold cysts and ligament vocal fold cysts involve similar symptoms.[1] The presence and the severity of symptoms may be influenced by the location and size of the cyst.[5] Common symptoms include:
- Hoarse voice
- Inability to produce high pitch notes
- Fatigue when speaking
- Limited pitch range
- Pain near the larynx
- Variations in pitch when speaking[1][5]
The accompanying signs and symptoms of vocal fold cysts may remain stable or increase over time.[1] In rare cases, symptoms actually improve.[1] Symptoms affecting the quality of the voice tend to worsen after speaking for long periods of time and when speaking with increased volume.[1] Many individuals who use their voice professionally will find even the presence of slight symptoms to be problematic.[1] However, some voice professionals are not impacted by the presence of vocal cysts.[6]
Diagnosis
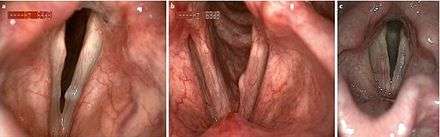
Mucous retention cysts are most commonly seen in individuals that endure high vocal stress in their daily lives, while epidermoid cysts are usually congenital or second to vocal trauma (see lead section for more information on different types of cysts).[5] The two types of vocal fold cysts can be differentiated from other vocal fold growths in several ways. Both types show decreased amplitude of vibrations and reduced or absent mucosal wave.[5] Mucous retention cysts show a translucent mass of mucous usually below the free margin of the glottis, while epidermoid cysts are yellow masses under the first epithelial layer of the vocal folds.[4] Epidermoid cysts generally appear in the superior and medial regions of the midmusculomembranous region of the folds, as opposed to mucous cysts appearing in the inferior region.[7] Vocal fold cysts are differentiated from other vocal fold masses in that they are unilateral and subepithelial.[7]
Four components to a full diagnosis are: medical and voice history, head and neck exam, then perceptual assessment of voice and imaging of vocal folds.[4] The primary perceptual sign of vocal fold cysts is hoarseness of the voice.[7] However, diagnosis is difficult; in most cases, when a diagnosis cannot first be reached via behavioural assessment and intervention, the patient undergoes an imaging procedure.[2] Imaging is most commonly done with laryngeal videostroboscopy.[4] This procedure provides information about vocal fold vibrations during speech, vocal intensity and vocal frequency.[4] Imaging shows the reduced movement of the vocal folds (mucosal wave) when a vocal fold cyst is present.[4]
Patients with vocal fold cysts are considered for surgery when presenting with:[2]
- Dysphonia
- Lack of improvement through voice therapy
Treatment
Vocal fold cysts are treated using a multidisciplinary approach.[8][9] Voice therapy to address harmful vocal behaviours is recommended as the first treatment option.[7] Voice therapy may involve reducing tension in the larynx, reducing loudness, reducing the amount of speech produced, and modifying the environment.[10] If symptoms are significant, treatment usually involves microsurgery to remove the cyst.[7]
During surgery, attempts are made to preserve as much vocal fold tissue as possible,[7] given that glottal insufficiency (a gap in the vocal folds) is a possible consequence of surgery.[8] Vocal fold tissue can be preserved during surgery by raising a microflap, removing the cyst, then laying the flap back down.[8] This is intended to lead to minimal scarring and improved voice function.[8] However, if any epithelium from the cyst sac is left behind during surgery, the cyst may regrow.[6] Surgery of the larynx may also be conducted using a CO2 laser, which was reported as early as the 1970s.[11] Congenital ductal cysts (those caused by blockage of a glandular duct) may be treated by marsupialization.[12]

Following surgery, patients are recommended to take 2 to 14 days of vocal rest.[2] In absolute vocal rest, activities such as talking, whispering, whistling, straining, coughing, and sneezing are restricted.[13] Once adequate healing has occurred, the patient may be transitioned to relative vocal rest, which typically involves 5 to 10 minutes of breathy voicing per hour.[13] Voice therapy is then required to restore as much function as possible.[7] Post-operative voice therapy may include addressing harmful vocal behaviours, exercises to restrengthen the larynx, and reintegration into normal voice activities.[14]
Professional voice users who do not experience substantial limitations due to their cysts may choose to forego surgery.[6] Considering that some cysts remain stable over long periods of time, voice therapy alone may be an option for those who are resistant to surgery.[8] Another option for those who are unwilling to undergo surgery is vocal fold steroid injection (VFSI).[15] Injection of the vocal folds may be done transorally or percutaneously, through the thyrohyoid membrane, thyroid cartilage, or cricothyroid membrane.[15] After VFSI, patients are recommended to take 1 to 7 days of vocal rest.[15] VFSI may also be used to delay surgery, or as a treatment method when the risks associated with surgery are deemed to be too high.[15]
Prognosis
Following diagnosis, voice therapy should be implemented to optimize vocal hygiene.[7] However, vocal fold cysts typically do not improve with solely vocal rest or vocal therapy. Instead, a surgical procedure utilizing the microflap approach is conducted to remove the cyst (see Treatment).
Following surgery, patients are advised to rest their voice for one week with gradual re-introduction of voice use with a Speech-Language Pathologist after this period of rest.[2] This initial rest period can vary between 2 and 14 days.[2] Patients with subepithelial cysts have a better prognosis for timely recovery of vocal abilities than patients with ligament vocal fold cysts.[2] Typically, patients can resume speaking activities in 7–30 days following surgery, and singing activities 30–90 days post-surgery.[2]
Up to 20% of patients show scarring, polyps or vascular changes of the vocal folds following surgery.[5] In severe cases, these resulting symptoms may require further surgery. The patient must always be aware of the impact and potential complications of surgery on their voice, especially if the voice is heavily used occupationally. In these cases, post-operative therapy should be discussed.
Prevention
A key aspect of preventing vocal fold cysts is good vocal hygiene.[16] Good vocal hygiene promotes the healthy use of the vocal apparatus and the avoidance of phonotrauma.[16] Good vocal hygiene practices involve the avoidance of:[16]
- Shouting
- Whispering loudly or for long periods of time
- Large quantities of talking over loud background noise
- Talking while yawning
- Continual clearing of the throat
- Speaking in an unnatural voice (i.e. too high or low)
- Talking with a cold or laryngitis
- Smoking tobacco or marijuana
- The consumption of alcohol and coffee
- The use of antihistamines, aspirin, steroids, tricyclic antidepressants, or any substance that alters perception (i.e. sleeping pills)
- Foul air[16]
In addition, good vocal hygiene involves getting enough rest and drinking lots of water.[16] It is important to keep the vocal fold tissue healthy and hydrated, and when possible to limit the quantity of speaking in order to avoid damage.[16]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Verdolini, Katherine; Rosen, Clark A; Branski, Ryan C (2005). Classification manual for voice disorders-I. Psychology Press.
- 1 2 3 4 5 6 7 8 Simpson, Blake; Rosen, Clark (2008). Operative Techniques in Laryngology. Berlin: Springer. ISBN 978-3-540-68107-6.
- 1 2 Reiter, Rudolf; Hoffman, Thomas Karl; Pickhard, Anja; Brosche, Sibylle (2015). "Hoarseness - Causes and Treatment". Deutsches Arzteblatt International. 112.
- 1 2 3 4 5 6 7 8 9 Johns, Michael M (2003). "Update on the etiology, diagnosis, and treatment of vocal fold nodules, polyps, and cysts". Current Opinion in Otolaryngology & Head and Neck Surgery. 11.
- 1 2 3 4 5 Bohlender, Jörg (2013). "Diagnostic and therapeutic pitfalls in benign vocal fold diseases". GMS Current Topics in Otorhinolaryngology Head and Neck Surgery. 12.
- 1 2 3 Altman, Kenneth W. "Vocal Fold Masses". Otolaryngologic Clinics of North America. 40 (5): 1091–1108. doi:10.1016/j.otc.2007.05.011.
- 1 2 3 4 5 6 7 8 Franco, Ramon A.; Andrus, Jennifer G. "Common Diagnoses and Treatments in Professional Voice Users". Otolaryngologic Clinics of North America. 40 (5): 1025–1061. doi:10.1016/j.otc.2007.05.008.
- 1 2 3 4 5 Costello, Declan; Sandhu, Guri, eds. (2016). Practical Laryngology. Boca Raton, FL: CRC Press, Taylor & Francis Group. ISBN 978-1-4441-8367-2.
- ↑ Lin, Fred Y.; Patel, Zara M., eds. (2014). ENT Board Prep: High Yield Review for the Otolaryngology In-service and Board Exams. New York, NY: Springer. ISBN 978-1-4614-8354-0.
- ↑ Colton, Raymond H.; Casper, Janina K.; Leonard, Rebecca (2006). Understanding Voice Problems: A Physiological Perspective for Diagnosis and Treatment. Baltimore: Lippincott Williams & Wilkins. ISBN 9780781742399.
- ↑ Benninger, Michael S. (2000). "Microdissection or Microspot CO2 Laser for Limited Vocal Fold Benign Lesions: A Prospective Randomized Trial". The Laryngoscope. 110 (S92). doi:10.1097/00005537-200002001-00001. ISSN 1531-4995.
- ↑ Ahmad, Sidrah M.; Soliman, Ahmed M.S. (February 2007). "Congenital Anomalies of the Larynx". Otolaryngologic Clinics of North America. 40 (1): 177–191. doi:10.1016/j.otc.2006.10.004.
- 1 2 Myers, Eugene N. (2008). Operative Otolaryngology: Head and Neck Surgery, Second Edition. Saunders. ISBN 978-1-4160-2445-3.
- ↑ Ballif, Catherine L.; Gorman, Stephen; Kelchner, Lisa N.; LeBorgne, Wendy D.; Rettig, Jennifer R. "Postsurgical Vocal Rest Recommendations" (PDF). Retrieved November 6, 2016.
- 1 2 3 4 Wang, Chi-Te; Liao, Li-Jen; Cheng, Po-Wen; Lo, Wu-Chia; Lai, Mei-Shu (2013). "Intralesional steroid injection for benign vocal fold disorders: A systematic review and meta-analysis". The Laryngoscope. 123 (1): 197–203. doi:10.1002/lary.23551. ISSN 1531-4995.
- 1 2 3 4 5 6 Calhoun, Karen H.; Wax, Mark K.; Ebling, David E., eds. (2001). Expert guide to otolaryngology (1st ed.). American College of Physicians.