Thrombosis prophylaxis
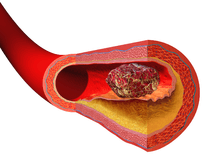
Thrombosis prophlaxis is the pre- and post-operative treatment to prevent the formation of blood clots inside a blood vessel, obstructing the flow of blood through the circulatory system. Limiting the flow through a blood vessel will cause hypoxia or tissue death. Blood clots can form in the body post-operative, most commonly in the legs.
Thrombosis prophlaxis is needed to prevent Venous stasis(VS). Venous stasis is a risk factor for forming blood clots in the deep veins of the legs.[1] Venous stasis can occur during the long periods of immobility that accompanies some surgeries. The use of intermittent pneumatic compression is common.[2][3]
Clarence Crafoord is credited with the first use of thrombosis prophylaxix in the 1930s.
Thrombosis prophylaxis is often prescribed for hospitalized patients routinely by a number of means. Pre-operatively some patients receive low-molecular-weight heparin once a day. Additional risk factors such as obesity, disease, malignancies, long surgeries, and immobility may influence the prescribed dosage. Anti-coagulant administration is often given before the start of the operation. There are concerns with the potential of increased risk of bleeding and so many surgeons start giving anti-coagulants the first 6 hours after surgery.[4]
Postoperative thrombosis prophylaxis remains a priority for most surgeons. Risk factors for developing thrombosis after surgery are pregnancy, age, contraceptive use, hormone replacement therapy, infection, malignant disease, venous insufficiency, obesity, heart failure, antipospholipid syndrome, and antithrombin deficiency.[4]
Intermittent pneumatic compression devices are used post-surgically to promote venous circulation.[5][6] Adding heparin to the use of compression stockings may prevent thrombosis.[7]
Physical thrombosis prophlaxis treatments are the implementation of early mobilization, physical therapy, patient education to teach the use of exercises, encouragement of the clinician to promote mobilization, and the fitting and use of high quality compression stockings.[4]
The Centers for Disease Control and Prevention recommend the following:
- Move around as soon as possible after having been confined to bed, such as after surgery, illness, or injury.
- If you’re at risk for DVT, talk to your doctor about:
- Graduated compression stockings (sometimes called “medical compression stockings”)
- Medication (anticoagulants) to prevent DVT.
- When sitting for long periods of time, such as when traveling for more than four hours:
- Get up and walk around every 2 to 3 hours.
- Exercise your legs while you’re sitting by:
- Raising and lowering your heels while keeping your toes on the floor
- Raising and lowering your toes while keeping your heels on the floor
- Tightening and releasing your leg muscles
- Wear loose-fitting clothes.
- You can reduce your risk by maintaining a healthy weight, avoiding a sedentary lifestyle, and following your doctor's recommendations based on your individual risk factors.[8]
Procedure
The application of antiembolism stockings (TED stockings) can be used prophylactically to prevent thrombosis. The procedure is not required to be aseptic, except for proper hand-washing techniques.[6]
Research
An international registry and risk assessment calculator is being used to centralize data on post-surgical venous thrombosis and its prevention.[9]
References
- ↑ Martinelli I, Bucciarelli P, Mannucci PM (2010). "Thrombotic risk factors: basic pathophysiology". Crit Care Med. 38 (2 Suppl): S3–9. doi:10.1097/CCM.0b013e3181c9cbd9. PMID 20083911.
- ↑ Hecht, M. E. (2010). A practical guide to hip surgery: from pre-op to recovery. Sunrise River Press. ISBN 978-1-934716-12-0.
- ↑ Gould MK, Garcia DA, Wren SM, et al. (2012). "Prevention of VTE in nonorthopedic surgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines". Chest. 141 (suppl 2): e227S–e277S. doi:10.1378/chest.11-2297. PMC 3278061
 . PMID 22315263.
. PMID 22315263. - 1 2 3 Abele, H (2014). Atlas of gynecologic surgery. Stuttgart: Thieme. ISBN 9783136507049; Access provided by the University of Pittsburgh
- ↑ Gould MK, Garcia DA, Wren SM, Karanicolas PJ, Arcelus JI, Heit JA, Samama CM (2012). "Prevention of VTE in Nonorthopedic Surgical Patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 suppl): e227S–e277S. doi:10.1378/chest.11-2297. PMC 3278061
 . PMID 22315263.
. PMID 22315263. - 1 2 Rosdahl, Caroline (2012). Textbook of basic nursing. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 9781605477725.
- ↑ Zareba, P; Wu, C; Agzarian, J; Rodriguez, D; Kearon, C (Aug 2014). "Meta-analysis of randomized trials comparing combined compression and anticoagulation with either modality alone for prevention of venous thromboembolism after surgery.". The British journal of surgery. 101 (9): 1053–62. doi:10.1002/bjs.9527. PMID 24916118.
- ↑ "Venous Thromboembolism (Blood Clots) Facts". Division of Blood Disorders National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention. 24 February 2016. Retrieved 2016-07-19.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "Computerized Registry of Patients with Veneous Thromboembolism - RIETE Registry". S & H Medical Science Service. Retrieved 2016-02-13.