Protein losing enteropathy
| Protein losing enteropathy | |
|---|---|
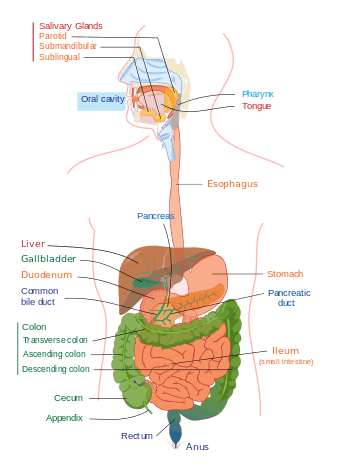
Upper and Lower human gastrointestinal tract
| |
| Protein losing enteropathy affects the GI tract[1] | |
| Classification and external resources | |
| ICD-10 | K90.4 |
| ICD-9-CM | 579.8 |
| OMIM | 226300 |
| DiseasesDB | 10811 |
| MedlinePlus | 002277 |
| eMedicine | med/1926 ped/1909 |
| MeSH | D011504 |
Protein losing enteropathy refers to any condition of the gastrointestinal tract (e.g. damage to the gut wall) that results in a net loss of protein from the body.[2]
Signs and symptoms
The signs/symptoms of protein losing enteropathy are consistent with diarrhea, fever, and general abdominal discomfort.[2] Swelling of the legs due to peripheral edema can also occur, however if the PLE is related to a systemic disease such as congestive heart failure or constrictive pericarditis, then the symptoms could be of the primary disease development.[3]
Causes
The causes of protein-losing enteropathy can include GI conditions (among other causes), like the following:[1]
- Inflammatory bowel disease.
- Idiopathic ulcerative jejunoileitis.
- Infection (secondary obstruction)
- Neoplasm (secondary obstruction)
- Sarcoidosis (secondary obstruction).
- Amyloidosis.
- Systemic lupus erythematosus (SLE).
- Ménétrier's disease.
- Zollinger-Ellison syndrome.
- Eosinophilic gastroenteritis.
- Coeliac disease.
- Primary intestinal lymphangectasia
Mechanism
The pathophysiology of protein losing enteropathy is a result of plasma proteins loss, which enters GI tract (lumen).[3] PLE is a complication of a disorder, be it lymphatic obstruction or mucosal injury.[4]
In pediatric protein losing enteropathy there are several changes in epithelial cells causing PLE by augmenting the rate of flow of proteins (serum). Congenital molecular abnormalities, or dysfunctional lymphatic drainage might cause epithelial matrix changes. Proteoglycans, which are glycosaminoglycan chains attached to protein, directly causes PLE, as well as, augments inflammatory cytokines. Children who have congenital glycosylation defects usually have protein losing enteropathy.[5][6]
Diagnosis
The diagnosis of protein-losing enteropathy is made by excluding other causes of protein loss. Endoscopy can be used to localize the cause of the protein loss in the bowel. Different methods include faecal excretion of alpha 1-antitrypsin which is a marker of protein-losing enteropathy, as well as, viral serologies which may be useful to detect PLE.[1]
Treatment
Treatment for protein losing enteropathy depends upon the underlying condition, according to Rychik, et al this could mean treatment of hypoproteinemia or of the intestinal mucosa.[7]
In terms of treatment for PLE after the Fontan operation treatment must be equal to the level of hypoproteinemia present. Therefore, it is useful to categorize patients based on their serum albumin levels, if less than normal (typically less than 3.5 g/dL) but greater than 2.5 g/dL, this can be seen as a mild form of protein losing enteropathy. Symptomatic management of edema with furosemide (and aldactone) can provide relief for the individual with mild hypoproteinemia.[8][9]
References
- 1 2 3 "Protein-losing Enteropathy. PLE information. What is PLE? | Patient". Patient. Retrieved 2016-02-19.
- 1 2 "Protein-losing enteropathy: MedlinePlus Medical Encyclopedia". www.nlm.nih.gov. Retrieved 2015-12-16.
- 1 2 "Protein-Losing Enteropathy: Background, Pathophysiology, Etiology".
- ↑ Wyllie, Robert; Hyams, Jeffrey S.; Kay, Marsha (2015-08-03). Pediatric Gastrointestinal and Liver Disease. Elsevier Health Sciences. p. 389. ISBN 9780323240994.
- ↑ Iozzo, Renato V.; Schaefer, Liliana (2015-03-01). "Proteoglycan form and function: A comprehensive nomenclature of proteoglycans". Matrix Biology. 42: 11–55. doi:10.1016/j.matbio.2015.02.003. – via ScienceDirect (Subscription may be required or content may be available in libraries.)
- ↑ "Pediatric Protein-Losing Enteropathy: Background, Pathophysiology, Epidemiology".
- ↑ Rychik, Jack; Spray, Thomas L. (2002-01-01). "Strategies to treat protein-losing enteropathy". Seminars in Thoracic and Cardiovascular Surgery: Pediatric Cardiac Surgery Annual. 5 (1): 3–11. doi:10.1053/pcsu.2002.31498. – via ScienceDirect (Subscription may be required or content may be available in libraries.)
- ↑ Rychik, Jack (2007-09-01). "Protein-Losing Enteropathy after Fontan Operation". Congenital Heart Disease. 2 (5): 288–300. doi:10.1111/j.1747-0803.2007.00116.x. ISSN 1747-0803.
- ↑ Topol, Eric J.; Califf, Robert M. (2007-01-01). Textbook of Cardiovascular Medicine. Lippincott Williams & Wilkins. p. 519. ISBN 9780781770125.
Further reading
- Umar, Sarah B.; DiBaise, John K. (2009-09-29). "Protein-Losing Enteropathy: Case Illustrations and Clinical Review". The American Journal of Gastroenterology. 105 (1): 43–49. doi:10.1038/ajg.2009.561. ISSN 0002-9270.
- Nikolaidis, Nikolaos; Tziomalos, Konstantinos; Giouleme, Olga; Gkisakis, Dimitrios; Kokkinomagoulou, Amalia; Karatzas, Nikolaos; Papanikolaou, Athanassios; Tsitourides, Ioannis; Eugenidis, Nikolaos (2005-10-01). "Protein-Losing Enteropathy as the Principal Manifestation of Constrictive Pericarditis". Journal of General Internal Medicine. 20 (10): C5–C7. doi:10.1111/j.1525-1497.2005.0202.x. ISSN 0884-8734. PMC 1490237
 . PMID 16191147.
. PMID 16191147.