Intraocular lens
| Intraocular lens | |
|---|---|
| Intervention | |
 | |
| ICD-9-CM | 13.72 |
| MeSH | D054120 |
| OPS-301 code | 5-984 |
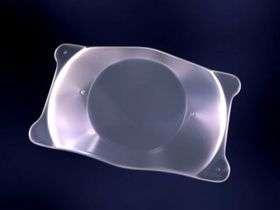
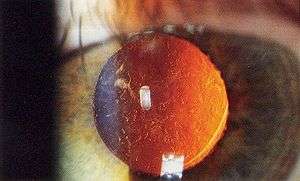
Intraocular lens (IOL) is a lens implanted in the eye used to treat cataracts or myopia. The most common type of IOL is the pseudophakic IOL. These are implanted during cataract surgery, after the cloudy crystalline lens (otherwise known as a cataract) has been removed. The pseudophakic IOL replaces the original crystalline lens, and provides the light focusing function originally undertaken by the crystalline lens. The second type of IOL, more commonly known as a phakic intraocular lens (PIOL), is a lens which is placed over the existing natural lens, and is used in refractive surgery to change the eye's optical power as a treatment for myopia, or nearsightedness.[1] IOLs usually consist of a small plastic lens with plastic side struts, called haptics, to hold the lens in place within the capsular bag inside the eye.[2] IOLs were conventionally made of an inflexible material (PMMA), although this has largely been superseded by the use of flexible materials. Most IOLs fitted today are fixed monofocal lenses matched to distance vision. However, other types are available, such as multifocal IOLs which provide the patient with multiple-focused vision at far and reading distance, and adaptive IOLs which provide the patient with limited visual accommodation.
Insertion of an intraocular lens for the treatment of cataracts is the most commonly performed eye surgical procedure. Surgeons annually implant more than 6 million lenses.[3] The procedure can be done under local anesthesia with the patient awake throughout the operation. The use of a flexible IOL enables the lens to be rolled for insertion into the capsule through a very small incision, thus avoiding the need for stitches, and this procedure usually takes less than 30 minutes in the hands of an experienced ophthalmologist. The recovery period is about 2–3 weeks. After surgery, patients should avoid strenuous exercise or anything else that significantly increases blood pressure. They should also visit their ophthalmologists regularly for several months so as to monitor the implants.
IOL implantation carries several risks associated with eye surgeries, such as infection, loosening of the lens, lens rotation, inflammation and night time halos, but a systematic review of studies has determined that the procedure is safer than conventional laser eye treatment.[4] Though IOLs enable many patients to have reduced dependence on glasses, most patients still rely on glasses for certain activities, such as reading.
Medical uses
Intraocular lenses have been used since 1999 for correcting larger errors in near-sighted, far-sighted, and astigmatic eyes. This type of IOL is also called phakic intraocular lens (PIOL), and the crystalline lens is not removed.
Phakic IOL appear to be less dangerous than excimer laser surgery in those with significant nearsightedness.[5]
More commonly, aphakic IOLs (that is, not PIOLs) are implanted via Clear Lens Extraction and Replacement (CLEAR) surgery. During CLEAR, the crystalline lens is extracted and an IOL replaces it in a process that is very similar to cataract surgery: both involve lens replacement, local anesthesia, both last approximately 30 minutes, and both require making a small incision in the eye for lens insertion. People recover from CLEAR surgery 1–7 days after the operation. During this time, they should avoid strenuous exercise or anything else that significantly raises blood pressure. They should also visit their ophthalmologists regularly for several months so as to monitor the IOL implants. CLEAR has a 90% success rate (risks include wound leakage, infection, inflammation, and astigmatism). CLEAR can only be performed on patients ages 40 and older. This is to ensure that eye growth, which disrupts IOL lenses, will not occur post-surgery.
Once implanted, IOL lenses have three major benefits. First, they are an alternative to LASIK, a form of eye surgery that does not work for people with serious vision problems. Effective IOL implants also entirely eliminate the need for glasses or contact lenses post-surgery for most patients. The cataract will not return, as the lens has been removed. The disadvantage is that the eye's ability to change focus (accommodate) has generally been reduced or eliminated, depending on the kind of lens implanted.
Some of the risks that FDA have been found so far during a three-year study of the Artisan are:
- a yearly loss of 1.8% of the endothelial cells,
- 0.6% risk of retinal detachment,
- 0.6% risk of cataract (other studies have shown a risk of 0.5 – 1.0%), and
- 0.4% risk of corneal swelling.
Other risks include:
- 0.03 – 0.05% eye infection risk, which in worst case can lead to blindness. This risk exists in all eye surgery procedures, and is not unique for IOLs.
- glaucoma,
- astigmatism,
- remaining near or far sightedness,
- rotation of the lens inside the eye within one or two days after surgery.
One of the causes of the risks above is that the lens can rotate inside the eye, if the PIOL is too short if the eye was incorrectly measured, or because the sulcus has a slightly oval shape (the height is slightly smaller than the width). Toric IOLs must be powered and aligned inside the eye on a meridian that corrects the patient's preexisting astigmatism. Again, these lenses can rotate inside the eye postoperatively, or be placed incorrectly by the operating surgeon. Either way, the patient's preexisting astigmatism may not be corrected completely or may even increase. When IOLs are implanted in the aphakic patient—either after clear lensectomy for the correction of refractive error or after cataract extraction to restore eyesight—astigmatism in these patients is mainly attributable to the cornea. The surgeon can ascertains the astigmatic, or steepest, meridian in a number of ways, including manifest refraction or corneal topography. Manifest refraction is the familiar test where the eye doctor rotates various lenses in front of the eye, asking the patient, "Which is better (or clearer), this one or this one?" Corneal topography is considered a more quantitative test, and for purposes of aligning a toric IOL, most surgeons use a measurement called simulated keratometry (SimK), which is calculated by the internal programming of the corneal topography machine, to determine the astigmatic meridian on the surface of the cornea. The astigmatic meridian can also be identified using corneal wavefront technology or paraxial curvature matching.
Accommodating IOLs
One of the major disadvantages of conventional IOLs is that they are primarily focused for distance vision. Though patients who undergo a standard IOL implantation no longer experience clouding from cataracts, they are unable to accommodate, or change focus from near to far, far to near, and to distances in between. Accommodating IOLs interact with ciliary muscles and zonules, using hinges at both ends to “latch on” and move forward and backward inside the eye using the same mechanism as normal accommodation. These IOLs have a 4.5-mm square-edged optic and a long hinged plate design with polyimide loops at the end of the haptics. The hinges are made of an advanced silicone called BioSil that was thoroughly tested to make sure it was capable of unlimited flexing in the eye.[6]
Evidence
- In a September 2004 FDA trial involving 325 patients:[7]
- 100% could see at intermediate distances (24" to 30") without glasses; the distance for most of life's activities
- 98.4% could see well enough to read the newspaper and the phone book without glasses.
- Some patients did require glasses for some tasks after implantation of the crystalens
- Vision was restored to 20/40 or better in 88% of patients compared to 35.9% of patients who received normal IOLs.
- In 2006, a 12-month study by Cummings et al. investigated contrast sensitivity and near visual acuity in patients who had received a Crystalens AT-45 versus those who received a standard IOL. Effectiveness was measured in terms of near, intermediate, and distance visual acuities and safety was evaluated by assessing complications. The study concluded that contrast sensitivity was not reduced compared to those receiving standard IOLs and provided good visual acuity at all distances in pseudophakic patients. There were no adverse complications reported. However, this study lacked a long-term follow up.[8]
- Pepose et al. (2007) tested the combination of a multifocal IOL in one eye and an accommodating IOL in the other eye. The group found that any combination of Crystalens in one or both eyes was better for intermediate vision. ReSTOR (multifocal IOL) is better for near vision. The Crystalens and ReSTOR combination had better mean intermediate and near vision overall.[9]
- Macsai et al. (2006) conducted a multicenter, nationwide study evaluating the visual outcomes of 112 cataract patients implanted with Crystalens IOL (n=56) versus standard monofocal IOLs (n=56). The Crystalens group demonstrated significantly better visual acuity compared to the monofocal patient group, as well as better distance and near vision 6 months post-operation.[10]
- In overall FDA clinical results on uncorrected binocular vision in 124 patients, 92 per cent had distance vision of 20/25 or better, 98 per cent had intermediate vision of 20/25 or better, and 73 per cent had near vision of 20/25 or better 11 to 15 months after surgery. In addition, 73.5 per cent either did not wear spectacles or wore them most none of the time.
- Sanders et al. (2007) published visual performance results after Tetraflex accommodative intraocular lens implantation. They found that 6 months post-operatively, all patients had at least 1 diopter of accommodative amplitude. At 6 months, 92.2 per cent of eyes had 20/40 or better uncorrected distance visual acuity (UCDVA) and 50.6 per cent of eyes achieved 20/20 or better UCDVA. At near, 48.1 per cent of eyes achieved 20/40 or better uncorrected near visual acuity.[11]
- A 2014 Cochrane review found that in adults with a history of uveitis, eyes treated with hydrophobic acrylic IOLs were 2 times more likely to have a best-corrected visual acuity (BCVA) of 20/40 or more when compared to eyes treated with silicone IOLs.[12]
Criticisms
- The main concern with accommodating IOLs is that there are no long-term, large-scale studies involving their use in patients. Such clinical studies using objective measurement techniques must be done to fully support the claim that accommodating IOLs can restore accommodative vision to the presbyopic eye.[13]
- Though it is rare, potential complications include capsular bag contraction and posterior capsule opacification.
- Further complications include permanent or temporary blindness, infection, hemorrhaging, and dislocation.[14]
- Dislocation requires additional surgeries to attach the Crystalens. Lens replacement surgery may involve additional risk especially for those with chronic health conditions such as high blood pressure.[14]
Materials

The various materials which have been used to manufacture intraocular lens implants include polymethylmethacrylate (PMMA), silicone, hydrophobic acrylate, hydrophilic acrylate and collamer.[15] Polymethylmethacrylate (PMMA) was the first material to be used successfully in intraocular lenses. British ophthalmologist Sir Harold Ridley observed that Royal Air Force pilots who sustained eye injuries during World War II involving PMMA windshield material did not show any rejection or foreign body reaction. Deducing that the transparent material was inert and useful for implantation in the eye, Ridley designed and implanted the first intraocular lens in a human eye.
Advances in technology have brought about the use of silicone and acrylic, both of which are soft foldable inert materials. This allows the lens to be folded and inserted into the eye through a smaller incision. Specifically, acrylic lenses are a better choice in people who have a history of uveitis, or are likely to have to undergo retinal surgery requiring vitrectomy with replacement by silicone oil, such as persons with proliferative diabetic retinopathy or who are at high risk of retinal detachment, such as persons with high myopia.
The trademarked "Natural Yellow" material is available in three hydrophilic IOLs. Dr. Patrick H. Benz of Benz Research and Development created the first IOL material to incorporate the same UV-A blocking and violet light filtering chromophore that's present in the human crystalline lens. This breakthrough material provides the exact chromophore the human retina naturally has for light protection.
Other IOLs include:
- Blue Light Filtering IOLs filter the UV and high-energy blue light present in natural and artificial light, both of which can cause vision problems; however too much filtering of blue light can increase depression, especially in the winter months (SAD).
- Toric IOLs (1998) correct astigmatic vision.
Types
- Phakia is the presence of the natural crystalline lenses.
- Aphakia is the absence of the natural crystalline lens. The aphakic state is usually due to surgery to remove a cataractous lens, but post-surgical aphakia is rare nowadays because of the ubiquity of intraocular lenses. Rarely, aphakia can be post-traumatic or congenital in nature.
- Pseudophakia is the substitution of the natural crystalline lens with an IOL, as is often done after cataract extraction or to correct refractive error.
The root of these words comes from the Greek word phakos 'lens'.[16]
Phakic IOLs are implanted without removal of the patient's original crystalline lens, and this is performed solely to correct refractive error in the presence of a clear crystalline lens.
Aphakic IOLs generally refer to lenses implanted secondarily in an eye already aphakic from previous surgery or trauma some time ago.
Pseudophakic IOLs refer to lenses implanted during cataract surgery, as a sequential step after removal of the cataractous lens of the person.
Many aphakic and pseudophakic IOLs such as anterior chamber IOLs or 3 piece posterior chamber IOLs can be used interchangeably. The exception are one piece IOLs, which must be placed within the capsular bag at the time of cataract surgery and hence cannot be used as secondary implants.
PIOLs
As with IOLs inserted after cataract extraction, phakic IOLs (PIOLs) can be either spheric or toric. The difference is that they are placed in an eye that retains the natural human crystalline lens. As with aphakic eyes, toric PIOLs have to be aligned with the meridian of astigmatism; toric IOL misalignment or rotation can lead to residual or even greater astigmatism postoperatively.
Depending on their placement site in the eye, PIOLs can be divided into:[16]
- Angle-supported PIOLs: those IOLs are placed in the anterior chamber. They are notorious for their negative impact on the corneal endothelial lining, which is vital for maintaining a healthy clear cornea.
- Iris-supported PIOLs: The IOL is attached by claws to the mid-peripheral iris by a technique called enclavation. It is believed to have a lesser effect on corneal endothelium. The main complication with this type is their tendency to cause endothelial cell reduction.
- Sulcus-supported PIOLs: this type is gaining more and more popularity. These IOLs are placed in the posterior chamber in front of the natural crystalline lens. They have special vaulting so as not to be in contact with the normal lens. The main complication with older versions was a small possibility of cataract formation.
Pseudophakic IOLs that address presbyopia
In the United States, a new category of intraocular lenses was opened with the approval by the Food and Drug Administration in 2003 of multifocal and accommodating lenses. These come at an additional cost to the recipient beyond what Medicare will pay and each has advantages and disadvantages.
New FDA-approved multifocal intraocular lens implants allow most postoperative cataract patients the advantage of glass-free vision. These new multifocal lenses are not a covered expense under most insurance plans (In the United States, Medicare decided to stop covering them in May 2005) and can cost the patient upwards of $2800 per eye. Latest advances include IOLs with square-edge design, non-glare edge design and yellow dye added to the IOL.
Multifocal IOLs – provide for simultaneous viewing of both distance vision and near vision. Some patients report glare and halos at night time with these lenses.
Accommodating IOLs – allow for both distance vision and midrange near vision. These IOLs are typically not as strong for closer vision as the multifocal IOLs.
To incorporate the strengths of each type of IOL, some eye surgeons recommend using a multifocal IOL in one eye to emphasize close reading vision and an accommodating IOL in the other eye for further midrange vision. This is called "mix and match." Distance vision is not compromised with this approach, while near vision is optimized.
History
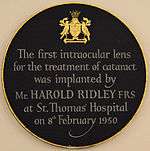
Sir Harold Ridley was the first to successfully implant an intraocular lens on 29 November 1949, at St Thomas' Hospital at London.[17] That first intraocular lens was manufactured by the Rayner company of Brighton, East Sussex, England from Perspex CQ Polymethylmethacrylate (PMMA) made by ICI (Imperial Chemical Industries). It is said the idea of implanting an intraocular lens came to him after an intern asked him why he was not replacing the lens he had removed during cataract surgery. The acrylic plastic material was chosen because Ridley noticed it was inert after seeing RAF (Royal Air Force) pilots of World War II with pieces of shattered canopies in their eyes (this acrylic resin is known by several trade names including Lucite and Plexiglas). The intraocular lens did not find widespread acceptance in cataract surgery until the 1970s, when further developments in lens design and surgical techniques had come about. As of the early 2000s, more than a million IOLs are implanted annually in the United States. That number was estimated by the World Health Organization to have increased to 20 million annually worldwide by 2010 (for cataract surgery), and has projected increased IOL surgeries to reach 32 million worldwide by 2020.[18]
See also
References
- ↑ Güell, Jose Luis; Morral, Merce; Kook, Daniel; Kohnen, Thomas (2010). "Phakic intraocular lenses". Journal of Cataract & Refractive Surgery. 36 (11): 1976–1993. doi:10.1016/j.jcrs.2010.08.014.
- ↑ Sanders, Donald; Vukich, John A (2006). "Comparison of Implantable Collamer Lens (ICL) and Laser-assisted in Situ Keratomileusis (LASIK) for Low Myopia". Cornea. 25 (10): 1139–46. doi:10.1097/ICO.0b013e31802cbf3c. PMID 17172886.
- ↑ Gaudet, Jodie ed. 1001 Inventions That Changed the World, page 697, ISBN 978-0-7333-2536-6
- ↑ Barsam A, Allan BD (2012). "Excimer laser refractive surgery versus phakic intraocular lenses for the correction of moderate to high myopia". Cochrane Database of Systematic Reviews. 1 (1): CD007679. doi:10.1002/14651858.CD007679.pub3. PMID 22258972.
- ↑ Barsam, A; Allan, BD (17 June 2014). "Excimer laser refractive surgery versus phakic intraocular lenses for the correction of moderate to high myopia.". The Cochrane database of systematic reviews. 6: CD007679. doi:10.1002/14651858.CD007679.pub4. PMID 24937100.
- ↑ Slade, Stephen. "Accommodating IOLs: Design, Technique, Results." Review of Ophthalmology. 2005. 20 Mar 2009. <http://www.revophth.com/index.asp?page=1_751.htm>
- ↑ United States Food and Drug Administration. Center for Devices and Radiological Health (CDRH). Crystalens Model AT-45 Accommodating IOL P030002. New Device Approval. CDRH Consumer Information. Updated 21 Jan 2004. http://web.archive.org/http://fda.gov/cdrh/mda/docs/p030002.html
- ↑ Cummings; et al. (May 2006). "Clinical evaluation of the Crystalens AT-45 accommodating interocular lens Results of the U.S. Food and Drug Administration clinical trial". J Cataract Refract Surg. 32 (5): 812–25.
- ↑ Pepose JS, Qazi MA, Davies J, Doane JF, Loden JC, Sivalingham V, Mahmoud AM. Visual performance of patients with bilateral vs combination Crystalens, ReZoom, and ReSTOR intraocular lens implants. Am J Ophthalmol. 2007 Sep: 144 (3) 347–357.
- ↑ Macsai; et al. (Apr 2006). "Visual outcomes after accommodating intraocular lens implantation". J Cataract Refract Surg. 32 (4): 628–33. doi:10.1016/j.jcrs.2006.01.027.
- ↑ Sanders DR, Sanders ML (2007). "Visual performance results after Tetraflex accommodating intraocular lens implantation". Ophthalmology. 114: 1679–1684. doi:10.1016/j.ophtha.2006.12.017.
- ↑ Leung TG, Lindsley K, Kuo IC (2014). "Types of intraocular lenses for cataract surgery in eyes with uveitis". Cochrane Database Syst Rev. 3: CD007284. doi:10.1002/14651858.CD007284.pub2. PMC 4261623
 . PMID 24590672.
. PMID 24590672. - ↑ Glasser Adrian (Feb 2006). "Restoration of accommodation". Current Opinion in Ophthalmology. 17 (1): 12–8. doi:10.1097/01.icu.0000193069.32369.e1.
- 1 2 Mahootchi, Ahad. "What Happens During a Crystalens Procedure?". The Eye Clinic of Florida. Retrieved 23 July 2014.
- ↑ Belluci R. An Introduction to Intraocular Lenses: Material, Optics, Haptics, Design and Aberration. In: Güell JL (ed): Cataract. ESASO Course Series. Basel, Karger, 2013, vol 3, pp 38–55
- 1 2 Myron Yanoff; Jay S. Duker (2009). Ophthalmology (3rd ed.). Mosby Elsevier. ISBN 978-0-323-04332-8.
- ↑ Ophthalmol, J. (2001). "Sir Harold Ridley's vision" (PDF). Br J Ophthalmol. 85: 1022–3. doi:10.1136/bjo.85.9.1022. PMC 1724118
 . PMID 11520745.
. PMID 11520745. - ↑ "The Global Intraocular Lens Market is Forecast to Reach $3.1 Billion b | ASDReports". www.asdreports.com. Retrieved 2015-09-14.