Fetus
| Part of a series on |
| Human growth and development |
|---|
 |
| Stages |
| Biological milestones |
| Development and psychology |
|
In human development, a fetus or foetus (/ˈfiːtəs/; plural fetuses or foetuses) is a prenatal human between the embryonic state and birth. The fetal stage of development tends to be taken as beginning at the gestational age of eleven weeks, i.e. nine weeks after fertilization.[1][2] In biological terms, however, prenatal development is a continuum, with no clear defining feature distinguishing an embryo from a fetus. The use of the term "fetus" generally implies that an embryo has developed to the point of being recognizable as a human; this is the point usually taken to be the ninth week after fertilization. A fetus is also characterized by the presence of all the major body organs, though they will not yet be fully developed and functional and some not yet situated in their final anatomical location.
Etymology
The word fetus (plural fetuses) is from the Latin fētus (“offspring”, “bringing forth”, “hatching of young”).[3][4][5] The British, Irish, and Commonwealth spelling is foetus, which has been in use since at least 1594.[6] It arose as a hypercorrection based on an incorrect etymology (i.e. due to insufficient knowledge of Latin) that may have originated with an error by Isidore of Seville in AD 620.[7][8] This spelling is the most common in most Commonwealth nations, except in the medical literature, where fetus is used. The etymologically accurate original spelling fetus is used in Canada and the United States. In addition, fetus is now the standard English spelling throughout the world in medical journals.[9] The spelling faetus was used historically.[10]
Development
Weeks 9 to 16 (2-1/4 to 4 months)

In humans, the fetal stage commences at the beginning of the ninth week.[1] At the start of the fetal stage, the fetus is typically about 30 millimetres (1.2 in) in length from crown to rump, and weighs about 8 grams.[1] The head makes up nearly half of the fetus' size.[11] Breathing-like movement of the fetus is necessary for stimulation of lung development, rather than for obtaining oxygen.[12] The heart, hands, feet, brain and other organs are present, but are only at the beginning of development and have minimal operation.[13][14] The genitalia of the fetus starts to form and placenta becomes fully functional during week 9.[15]
At this point in development, uncontrolled movements and twitches occur as muscles, the brain, and pathways begin to develop.[16]
Weeks 17 to 25 (4-1/4 to 6-1/4 months)
A woman pregnant for the first time (primiparous), typically feels fetal movements at about 21 weeks, whereas a woman who has given birth at least once (multiparous), will typically feel movements by 20 weeks.[17] By the end of the fifth month, the fetus is about 20 cm (8 inches) long.
Weeks 26 to 38 (6-1/2 to 9-1/2 months)

The amount of body fat rapidly increases. Lungs are not fully mature. Thalamic brain connections, which mediate sensory input, form. Bones are fully developed, but are still soft and pliable. Iron, calcium, and phosphorus become more abundant. Fingernails reach the end of the fingertips. The lanugo, or fine hair, begins to disappear, until it is gone except on the upper arms and shoulders. Small breast buds are present on both sexes. Head hair becomes coarse and thicker. Birth is imminent and occurs around the 38th week after fertilization. The fetus is considered full-term between weeks 36 and 40, when it is sufficiently developed for life outside the uterus.[19][20] It may be 48 to 53 cm (19 to 21 inches) in length, when born. Control of movement is limited at birth, and purposeful voluntary movements develop all the way until puberty.[21][22]
Variation in growth
There is much variation in the growth of the human fetus. When fetal size is less than expected, that condition is known as intrauterine growth restriction (IUGR) also called fetal growth restriction (FGR); factors affecting fetal growth can be maternal, placental, or fetal.[23]
Maternal factors include maternal weight, body mass index, nutritional state, emotional stress, toxin exposure (including tobacco, alcohol, heroin, and other drugs which can also harm the fetus in other ways), and uterine blood flow.
Placental factors include size, microstructure (densities and architecture), umbilical blood flow, transporters and binding proteins, nutrient utilization and nutrient production.
Fetal factors include the fetus genome, nutrient production, and hormone output. Also, female fetuses tend to weigh less than males, at full term.[23]
Fetal growth is often classified as follows: small for gestational age (SGA), appropriate for gestational age (AGA), and large for gestational age (LGA).[24] SGA can result in low birth weight, although premature birth can also result in low birth weight. Low birth weight increases risk for perinatal mortality (death shortly after birth), asphyxia, hypothermia, polycythemia, hypocalcemia, immune dysfunction, neurologic abnormalities, and other long-term health problems. SGA may be associated with growth delay, or it may instead be associated with absolute stunting of growth.
Viability
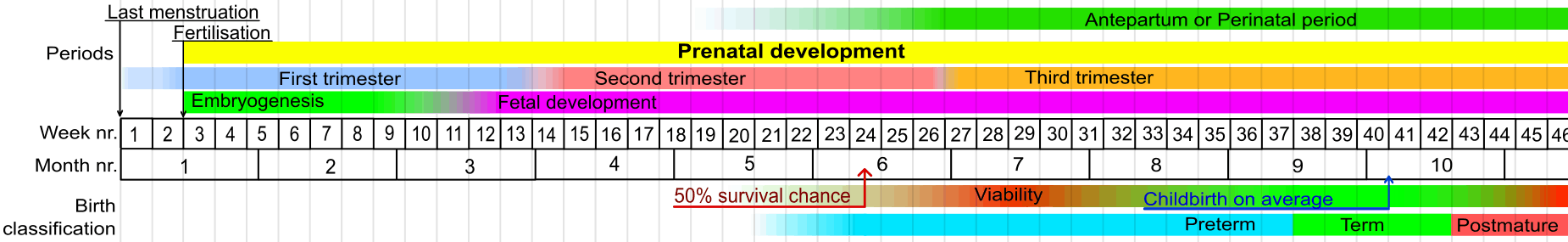
Viability refers to a point in fetal development at which the fetus may survive outside the womb. The lower limit of viability is approximately 5-3/4 months gestational age and is usually later.[25]
There is no sharp limit of development, age, or weight at which a fetus automatically becomes viable.[26] According to data from 2003–05, survival rates are 20–35% for babies born at 23 weeks of gestation (5-3/4 months); 50–70% at 24-25 weeks (6 - 6-1/4 months); and >90% at 26-27 weeks (6-1/2 - 6-3/4 months) and over.[27] It is rare for a baby weighing less than 1.1 pounds to survive.[26]
When such premature babies are born, the main causes of perinatal mortality are that the respiratory system and the central nervous system are not completely differentiated. If given expert postnatal care, some fetuses weighing less than 1.1 pounds may survive, and are referred to as extremely low birth weight or immature infants.[26] Preterm birth is the most common cause of perinatal mortality, causing almost 30 percent of neonatal deaths.[27]
Fetal pain
Fetal pain, its existence and its implications are debated politically and academically. According to the conclusions of a review published in 2005, "Evidence regarding the capacity for fetal pain is limited but indicates that fetal perception of pain is unlikely before the third trimester."[28][29] However, developmental neurobiologists argue that the establishment of thalamocortical connections (at about 6-1/2 months) is an essential event with regard to fetal perception of pain.[30] Nevertheless, the perception of pain involves sensory, emotional and cognitive factors and it is "impossible to know" when pain is experienced, even if it is known when thalamocortical connections are established.[30] Some authors [31] argue that fetal pain is possible from the second half of pregnancy: “The available scientific evidence makes it possible, even probable, that fetal pain perception occurs well before late gestation” wrote KJS Anand in the journal of the IASP.[32]
Whether a fetus has the ability to feel pain and suffering is part of the abortion debate.[33][34] In the United States, for example, pro-life advocates have proposed legislation that would require providers of abortions to inform women that their fetuses may feel pain during the procedure and that would require each woman to accept or decline anesthesia for the fetus.[35]
Circulatory system
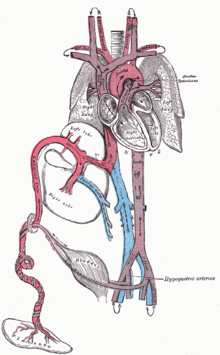
The heart and blood vessels which form the circulatory system, form relatively early during embryonic development, but continue to grow and develop in complexity in the growing fetus. A functional circulatory system is a biological necessity, since mammalian tissues can not grow more than a few cell layers thick without an active blood supply. The prenatal circulation of blood is different than the postnatal circulation, mainly because the lungs are not in use. The fetus obtains oxygen and nutrients from the mother through the placenta and the umbilical cord.[36]
Blood from the placenta is carried to the fetus by the umbilical vein. About half of this enters the fetal ductus venosus and is carried to the inferior vena cava, while the other half enters the liver proper from the inferior border of the liver. The branch of the umbilical vein that supplies the right lobe of the liver first joins with the portal vein. The blood then moves to the right atrium of the heart. In the fetus, there is an opening between the right and left atrium (the foramen ovale), and most of the blood flows from the right into the left atrium, thus bypassing pulmonary circulation. The majority of blood flow is into the left ventricle from where it is pumped through the aorta into the body. Some of the blood moves from the aorta through the internal iliac arteries to the umbilical arteries, and re-enters the placenta, where carbon dioxide and other waste products from the fetus are taken up and enter the woman's circulation.[36]
Some of the blood from the right atrium does not enter the left atrium, but enters the right ventricle and is pumped into the pulmonary artery. In the fetus, there is a special connection between the pulmonary artery and the aorta, called the ductus arteriosus, which directs most of this blood away from the lungs (which aren't being used for respiration at this point as the fetus is suspended in amniotic fluid).[36]
Postnatal development
With the first breath after birth, the system changes suddenly. Pulmonary resistance is reduced dramatically, prompting more blood to move into the pulmonary arteries from the right atrium and ventricle of the heart and less to flow through the foramen ovale into the left atrium. The blood from the lungs travels through the pulmonary veins to the left atrium, producing an increase in pressure that pushes the septum primum against the septum secundum, closing the foramen ovale and completing the separation of the newborn's circulatory system into the standard left and right sides. Thereafter, the foramen ovale is known as the fossa ovalis.
The ductus arteriosus normally closes within one or two days of birth, leaving the ligamentum arteriosum, while the umbilical vein and ductus venosus usually closes within two to five days after birth, leaving, respectively, the liver's ligamentum teres and ligamentum venosus.
Differences between fetal and postnatal
Remnants of the fetal circulation can be found in the adult.[37][38]
| Fetal | Developed |
|---|---|
| foramen ovale | fossa ovalis |
| ductus arteriosus | ligamentum arteriosum |
| extra-hepatic portion of the fetal left umbilical vein | ligamentum teres hepatis ("round ligament of the liver") |
| intra-hepatic portion of the fetal left umbilical vein (ductus venosus) |
ligamentum venosum |
| proximal portions of the fetal left and right umbilical arteries | umbilical branches of the internal iliac arteries |
| distal portions of the fetal left and right umbilical arteries | medial umbilical ligaments |
In addition to differences in circulation, the developing fetus also employs a different type of oxygen transport molecule in its hemoglobin from that when it is born and breathing its own oxygen. Fetal hemoglobin enhances the fetus' ability to draw oxygen from the placenta. Its oxygen-hemoglobin dissociation curve is shifted to the left, meaning that it is able to absorb oxygen at lower concentrations than adult hemoglobin. This enables fetal hemoglobin to absorb oxygen from adult hemoglobin in the placenta, where the oxygen pressure is lower than at the lungs. Until around six months' old, the human infant's hemoglobin molecule is made up of two alpha and two gamma chains (2α2γ). The gamma chains are gradually replaced by beta chains until the molecule becomes hemoglobin A with its two alpha and two beta chains (2α2β).

 Fetus at 4-1/4 months
Fetus at 4-1/4 months Fetus at 5 months
Fetus at 5 months
Immune system
The placenta functions as a maternal-fetal barrier against the transmission of microbes. When this is insufficient, mother-to-child transmission of infectious diseases can occur.
Maternal IgG antibodies cross the placenta, giving the fetus passive immunity against those diseases for which the mother has antibodies. This transfer of antibodies in humans begins as early as the fifth month (gestational age) and certainly by the sixth month.[39]
Developmental problems
A developing fetus is highly susceptible to anomalies in its growth and metabolism, increasing the risk of birth defects. One area of concern is the pregnant woman's lifestyle choices made during pregnancy.[40] Diet is especially important in the early stages of development. Studies show that supplementation of the woman's diet with folic acid reduces the risk of spina bifida and other neural tube defects. Another dietary concern is whether breakfast is eaten. Skipping breakfast could lead to extended periods of lower than normal nutrients in the woman's blood, leading to a higher risk of prematurity, or other birth defects in the fetus. During this time alcohol consumption may increase the risk of the development of fetal alcohol syndrome, a condition leading to intellectual disability in some infants.[41]
Smoking during pregnancy may also lead to reduced birth weight. Low birth weight is defined as 2500 grams (5.5 lb). Low birth weight is a concern for medical providers due to the tendency of these infants, described as "premature by weight", to have a higher risk of secondary medical problems. Some research shows that fetal ultrasounds (including Doppler, 3D/4D ultrasound and 2D ultrasound) can have negative effect on birth weight and neurodevelopment.[42]
Congenital anomalies are acquired before birth. Infants with certain congenital anomalies of the heart can survive only as long as the ductus remains open: in such cases the closure of the ductus can be delayed by the administration of prostaglandins to permit sufficient time for the surgical correction of the anomalies. Conversely, in cases of patent ductus arteriosus, where the ductus does not properly close, drugs that inhibit prostaglandin synthesis can be used to encourage its closure, so that surgery can be avoided.
Legal issues
Abortion of a human pregnancy is legal and/or tolerated in most countries, although with gestational time limits that normally prohibit late-term abortions.[43]
See also
References
- 1 2 3 Klossner, N. Jayne, Introductory Maternity Nursing (2005): "The fetal stage is from the beginning of the 9th week after fertilization and continues until birth"
- ↑ The American Pregnancy Association
- ↑ O.E.D.2nd Ed.2005
- ↑ Harper, Douglas. (2001). Online Etymology Dictionary. Retrieved 2007-01-20.
- ↑ "Charlton T. Lewis, An Elementary Latin Dictionary, fētus". Retrieved 2015-09-24.
- ↑ "Foetus". Oxford English Dictionary.
- ↑ Hamilton, W. J. (18 February 1967). "Foetus—or Fetus?". British Medical Journal. 1 (5537). PMC 1841520
 .
. - ↑ Aronson, Jeff (26 July 1997). "When I use a word...:Oe no!". British Medical Journal. 315 (7102). doi:10.1136/bmj.315.7102.0h. Retrieved 25 September 2012.
- ↑ New Oxford Dictionary of English.
- ↑ American Dictionary of the English Language, Noah Webster, 1828.
- ↑ MedlinePlus
- ↑ Institute of Medicine of the National Academies, Preterm Birth: Causes, Consequences, and Prevention (2006), page 317. Retrieved 2008-03-12
- ↑ The Columbia Encyclopedia (Sixth Edition). Retrieved 2007-03-05.
- ↑ Greenfield, Marjorie. “Dr. Spock.com". Retrieved 2007-01-20.
- ↑ "9 Weeks Pregnant – Symptoms, Fetal Development, Tips". Retrieved 2016-07-21.
- ↑ Prechtl, Heinz. "Prenatal and Early Postnatal Development of Human Motor Behavior" in Handbook of brain and behaviour in human development, Kalverboer and Gramsbergen eds., pp. 415-418 (2001 Kluwer Academic Publishers): "The first movements to occur are sideward bendings of the head....At 9-10 weeks postmestrual age complex and generalized movements occur. These are the so-called general movements (Prechtl et al., 1979) and the startles. Both include the whole body, but the general movements are slower and have a complex sequence of involved body parts, while the startle is a quick, phasic movement of all limbs and trunk and neck."
- ↑ Levene, Malcolm et al. Essentials of Neonatal Medicine (Blackwell 2000), p. 8. Retrieved 2007-03-04.
- ↑ "Fetal development - 40 weeks". http://www.babycentre.co.uk/. BabyCenter, L.L.C. 2015. Retrieved 26 August 2015. External link in
|website=(help) - ↑ Your Pregnancy: 36 Weeks BabyCenter.com Retrieved June 1, 2007.
- ↑ "full-term" defined by Memidex/WordNet.
- ↑ Stanley, Fiona et al. "Cerebral Palsies: Epidemiology and Causal Pathways", page 48 (2000 Cambridge University Press): "Motor competence at birth is limited in the human neonate. The voluntary control of movement develops and matures during a prolonged period up to puberty...."
- ↑ Becher, Julie-Claire. "Insights into Early Fetal Development"., Behind the Medical Headlines (Royal College of Physicians of Edinburgh and Royal College of Physicians and Surgeons of Glasgow October 2004)
- 1 2 Holden, Chris and MacDonald, Anita. Nutrition and Child Health (Elsevier 2000). Retrieved 2007-03-04.
- ↑ Queenan, John. Management of High-Risk Pregnancy (Blackwell 1999). Retrieved 2007-03-04.
- ↑ Halamek, Louis. "Prenatal Consultation at the Limits of Viability", NeoReviews, Vol.4 No.6 (2003): "most neonatologists would agree that survival of infants younger than approximately 22 to 23 weeks’ estimated gestational age [i.e. 20 to 21 weeks' estimated fertilization age] is universally dismal and that resuscitative efforts should not be undertaken when a neonate is born at this point in pregnancy."
- 1 2 3 Moore, Keith and Persaud, T. The Developing Human: Clinically Oriented Embryology, p. 103 (Saunders 2003).
- 1 2 March of Dimes - Neonatal Death, retrieved September 2, 2009.
- ↑ Lee, Susan; Ralston, HJ; Drey, EA; Partridge, JC; Rosen, MA (August 24–31, 2005). "Fetal Pain A Systematic Multidisciplinary Review of the Evidence". Journal of the American Medical Association. American Medical Association. 294 (8): 947–54. doi:10.1001/jama.294.8.947. PMID 16118385. Retrieved 2008-02-14. Two authors of the study published in JAMA did not report their abortion-related activities, which pro-life groups called a conflict of interest; the editor of JAMA responded that JAMA probably would have mentioned those activities if they had been disclosed, but still would have published the study. See Denise Grady, “Study Authors Didn't Report Abortion Ties”, New York Times (2005-08-26).
- ↑ "Study: Fetus feels no pain until third trimester" MSNBC
- 1 2 Johnson, Martin and Everitt, Barry. Essential reproduction (Blackwell 2000): "The multidimensionality of pain perception, involving sensory, emotional, and cognitive factors may in itself be the basis of conscious, painful experience, but it will remain difficult to attribute this to a fetus at any particular developmental age." Retrieved 2007-02-21.
- ↑ Glover V. The fetus may feel pain from 20 weeks. Conscience. 2004-2005 Winter;25(3):35-7
- ↑ http://www.iasp-pain.org/AM/AMTemplate.cfm?Section=HOME&TEMPLATE=/CM/ContentDisplay.cfm&CONTENTID=15390&SECTION=HOME
- ↑ White, R. Frank. " [[New research has discovered that unborn babies can feel pain. "The neural pathways are present for pain to be experienced quite early by unborn babies,” explains Steven Calvin, M.D., perinatologist, chair of the Program in Human Rights Medicine, University of Minnesota, where he teaches obstetrics." ]http://www.asahq.org/Newsletters/2001/10_01/white.htm Are We Overlooking Fetal Pain and Suffering During Abortion?]", American Society of Anesthesiologists Newsletter (October 2001). Retrieved 2007-03-10.
- ↑ David, Barry & and Goldberg, Barth. "Recovering Damages for Fetal Pain and Suffering", Illinois Bar Journal (December 2002). Retrieved 2007-03-10.
- ↑ Weisman, Jonathan. "House to Consider Abortion Anesthesia Bill", Washington Post 2006-12-05. Retrieved 2007-02-06.
- 1 2 3 Whitaker, Kent. Comprehensive Perinatal and Pediatric Respiratory Care (Delmar 2001). Retrieved 2007-03-04.
- ↑ Dudek, Ronald and Fix, James. Board Review Series Embryology (Lippincott 2004). Retrieved 2007-03-04.
- ↑ University of Michigan Medical School, Fetal Circulation and Changes at Birth. Retrieved 2007-03-04.
- ↑ Page 202 of Pillitteri, Adele (2009). Maternal and Child Health Nursing: Care of the Childbearing and Childrearing Family. Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 1-58255-999-6.
- ↑ Dalby, JT (1978). "Environmental effects on prenatal development". Journal of Pediatric Psychology. 3: 105–109. doi:10.1093/jpepsy/3.3.105.
- ↑ Streissguth, Ann Pytkowicz (1997). Fetal alcohol syndrome: a guide for families and communities. Baltimore, MD: Paul H Brookes Pub. ISBN 1-55766-283-5.
- ↑ http://www.midwiferytoday.com/articles/ultrasoundrodgers.asp
- ↑ Anika Rahman, Laura Katzive and Stanley K. Henshaw. "A Global Review of Laws on Induced Abortion, 1985-1997", International Family Planning Perspectives Volume 24, Number 2 (June 1998).
External links
| Wikimedia Commons has media related to Fetus. |
- Prenatal Image Gallery Index at the Endowment for Human Development website, featuring numerous motion pictures of human fetal movement.
- "In the Womb" (National Geographic video).
| Preceded by Embryo |
Stages of human development Fetus |
Succeeded by Infancy |