Ptosis (eyelid)
| Ptosis of the eyelids | |
|---|---|
 | |
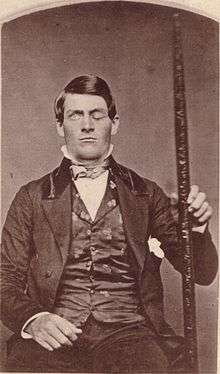
| Ptosis of the left eyelid (unilateral ptosis). A headshot daguerreotype of an unidentified male, by William Bell in 1852. | |
| Pronunciation | /ˈtoʊsɪs/ |
| Classification and external resources | |
| Specialty | Ophthalmology, neurology |
| ICD-10 | H02.4, Q10.0 |
| ICD-9-CM | 374.3 |
| DiseasesDB | 25466 |
| MedlinePlus | 001018 |
| eMedicine | oph/201 oph/345 |
| MeSH | D001763 |
Ptosis is a drooping or falling of the upper eyelid. The drooping may be worse after being awake longer, when the individual's muscles are tired. This condition is sometimes called "lazy eye", but that term normally refers to amblyopia. If severe enough and left untreated, the drooping eyelid can cause other conditions, such as amblyopia or astigmatism. This is why it is especially important for this disorder to be treated in children at a young age, before it can interfere with vision development. The term is from Greek πτῶσις "a fall, falling".
Causes
Ptosis occurs due to dysfunction of the muscles that raise the eyelid or their nerve supply (oculomotor nerve for levator palpebrae superioris and sympathetic nerves for superior tarsal muscle). It can affect one eye or both eyes and is more common in the elderly, as muscles in the eyelids may begin to deteriorate. One can, however, be born with ptosis. Congenital ptosis is hereditary in three main forms.[1] Causes of congenital ptosis remain unknown. Ptosis may be caused by damage/trauma to the muscle which raises the eyelid, damage to the superior cervical sympathetic ganglion or damage to the nerve (3rd cranial nerve (oculomotor nerve)) which controls this muscle. Such damage could be a sign or symptom of an underlying disease such as diabetes mellitus, a brain tumor, a pancoast tumor (apex of lung) and diseases which may cause weakness in muscles or nerve damage, such as myasthenia gravis or Oculopharyngeal muscular dystrophy. Exposure to the toxins in some snake venoms, such as that of the black mamba, may also cause this effect.
Ptosis can be caused by the aponeurosis of the levator muscle, nerve abnormalities, trauma, inflammation or lesions of the lid or orbit.[2] Dysfunctions of the levators may occur as a result of autoimmune antibodies attacking and eliminating the neurotransmitter.[3]
Ptosis may be due to a myogenic, neurogenic, aponeurotic, mechanical or traumatic cause and it usually occurs isolated, but may be associated with various other conditions, like immunological, degenerative, or hereditary disorders, tumors, or infections [4]
Acquired ptosis is most commonly caused by aponeurotic ptosis. This can occur as a result of senescence, dehiscence or disinsertion of the levator aponeurosis. Moreover, chronic inflammation or intraocular surgery can lead to the same effect. Also, wearing contact lenses for long periods of time is thought to have a certain impact on the development of this condition.
Congenital neurogenic ptosis is believed to be caused by the Horner syndrome.[2] In this case, a mild ptosis may be associated with ipsilateral ptosis, iris and areola hypopigmentation and anhidrosis due to the paresis of the Mueller muscle. Acquired Horner syndrome may result after trauma, neoplastic insult, or even vascular disease.
People of East Asian descent with epicanthic folds are more likely to have ptosis in their eyelids.
Ptosis due to trauma can ensue after an eyelid laceration with transection of the upper eyelid elevators or disruption of the neural input.[2]
Other causes of ptosis include eyelid neoplasms, neurofibromas or the cicatrization after inflammation or surgery. Mild ptosis may occur with aging. A drooping eyelid can be one of the first signals of a third nerve palsy due to a cerebral aneurysm, that otherwise is asymptomatic and referred to as an oculomotor nerve palsy.
Drugs
Use of high doses of opioid drugs such as morphine, oxycodone, heroin, or hydrocodone can cause ptosis.[5] Pregabalin (Lyrica), an anticonvulsant drug, has also been known to cause mild ptosis.[6]
Classification

Depending upon the cause it can be classified into:
- Neurogenic ptosis which includes oculomotor nerve palsy, Horner's syndrome, Marcus Gunn jaw winking syndrome, third cranial nerve misdirection.
- Myogenic ptosis which includes oculopharyngeal muscular dystrophy, myasthenia gravis, myotonic dystrophy, ocular myopathy, simple congenital ptosis, blepharophimosis syndrome
- Aponeurotic ptosis which may be involutional or post-operative
- Mechanical ptosis which occurs due to edema or tumors of the upper lid
- Neurotoxic ptosis which is a classic symptom of envenomation[7] by elapid snakes such as cobras,[8] kraits,[9] mambas and taipans. Bilateral ptosis is usually accompanied by diplopia, dysphagia and/or progressive muscular paralysis. Regardless, neurotoxic ptosis is a precursor to respiratory failure and eventual suffocation caused by complete paralysis of the thoracic diaphragm. It is therefore a medical emergency and immediate treatment is required. Similarly, ptosis may occur in victims of Botulism (caused by Botulinum toxin) and this is also regarded as a life-threatening symptom
- Pseudo ptosis due to:
- Lack of lid support: empty socket or atrophic globe.
- Higher lid position on the other side: as in lid retraction
Pathology

Myasthenia gravis is a common neurogenic ptosis which could be also classified as neuromuscular ptosis because the site of pathology is at the neuromuscular junction. Studies have shown that up to 70% of myasthenia gravis patients present with ptosis, and 90% of these patients will eventually develop ptosis.[10] In this case, ptosis can be unilateral or bilateral and its severity tends to be oscillating during the day, because of factors such as fatigue or drug effect. This particular type of ptosis is distinguished from the others with the help of a Tensilon challenge test and blood tests. Also, specific to myasthenia gravis is the fact that coldness inhibits the activity of cholinesterase, which makes possible differentiating this type of ptosis by applying ice onto the eyelids. Patients with myasthenic ptosis are very likely to still experience a variation of the drooping of the eyelid at different hours of the day.
The ptosis caused by the oculomotor palsy can be unilateral or bilateral, as the subnucleus to the levator muscle is a shared, midline structure in the brainstem. In cases in which the palsy is caused by the compression of the nerve by a tumor or aneurysm, it is highly likely to result in an abnormal ipsilateral papillary response and a larger pupil. Surgical third nerve palsy is characterized by a sudden onset of unilateral ptosis and an enlarged or sluggish pupil to the light. In this case, imaging tests such as CTs or MRIs should be considered. Medical third nerve palsy, contrary to surgical third nerve palsy, usually does not affect the pupil and it tends to slowly improve in several weeks. Surgery to correct ptosis due to medical third nerve palsy is normally considered only if the improvement of ptosis and ocular motility are unsatisfactory after half a year. Patients with third nerve palsy tend to have diminished or absent function of the levator.
When caused by Horner's syndrome, ptosis is usually accompanied by miosis and anhidrosis. In this case, the ptosis is due to the result of interruption innervations to the sympathetic, autonomic Muller's muscle rather than the somatic levator palpebrae superioris muscle. The lid position and pupil size are typically affected by this condition and the ptosis is generally mild, no more than 2 mm. The pupil might be smaller on the affected side. While 4% cocaine instilled to the eyes can confirm the diagnosis of Horner's syndrome, Hydroxyamphetamine eye drops can differentiate the location of the lesion.[10]
Chronic progressive external ophthalmoplegia is a systemic condition that occurs and which usually affects only the lid position and the external eye movement, without involving the movement of the pupil. This condition accounts for nearly 45% of myogenic ptosis cases. Most patients develop ptosis due to this disease in their adulthood. Characteristic to ptosis caused by this condition is the fact that the protective up rolling of the eyeball when the eyelids are closed is very poor.
Treatment
Aponeurotic and congenital ptosis may require surgical correction if severe enough to interfere with vision or if cosmetics is a concern. Treatment depends on the type of ptosis and is usually performed by an ophthalmic plastic and reconstructive surgeon, specializing in diseases and problems of the eyelid.
Surgical procedures include:
- Levator resection
- Müller muscle resection
- Frontalis sling operation (preferred option for oculopharyngeal muscular dystrophy)
Non-surgical modalities like the use of "crutch" glasses or Ptosis crutches or special scleral contact lenses to support the eyelid may also be used.
Ptosis that is caused by a disease may improve if the disease is treated successfully, although some related diseases, such as oculopharyngeal muscular dystrophy currently have no treatments or cures.
Etymology
Ptosis is derived from the Greek word (πτῶσις) “fall,” and is defined as the “abnormal lowering or prolapse of an organ or body part."
References
- ↑ "Congenital Ptosis". MEDgle. Retrieved 2008-10-20.
- 1 2 3 Adult Ptosis at eMedicine
- ↑ "Eye Ptosis Congenital". Retrieved 2010-06-14.
- ↑ Finsterer, J (2003). "Ptosis: causes, presentation, and management". Aesthetic Plastic Surgery. 27 (3): 193–204. doi:10.1007/s00266-003-0127-5. PMID 12925861.
- ↑ Iqbal N (2002). "Ptosis, convergence disorder and heroin" (PDF). Annals of Saudi Medicine. 22 (5–6): 369–71. PMID 17146268.
- ↑ "Lyrica (Pregabalin) – Reports of Side Effects & Adverse Reactions". DrugLib.com. Retrieved 2010-07-12.
- ↑ Warrell, D. A.; Hudson, B. J.; Lalloo, D. G.; Trevett, A. J.; Whitehead, P; Bamler, P. R.; Ranaivoson, M; Wiyono, A; Richie, T. L.; Fryauff, D. J.; O'Shea, M. T.; Richards, A. M.; Theakston, R. D. (1996). "The emerging syndrome of envenoming by the New Guinea small-eyed snake Micropechis ikaheka". QJM : monthly journal of the Association of Physicians. 89 (7): 523–30. doi:10.1093/qjmed/89.7.523. PMID 8759493.
- ↑ "Nature's poisons". Science Museum (London). Retrieved 2008-10-21.
- ↑ "Management of Snake bites in South East Asia – Part 2". World Health Organization. Retrieved 2008-10-12.
- 1 2 "Ptosis" (PDF). Retrieved 2010-06-14.
Further reading
- The AMA Medical Guide, Random House, Inc. New York, 1997 ed.
External links
- Finsterer, Josef (2003). "Ptosis: Causes, Presentation, and Management". Aesthetic Plastic Surgery. 27 (3): 193–204. doi:10.1007/s00266-003-0127-5. PMID 12925861.