Clotrimazole
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Desenex, Canesten, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682753 |
| Pregnancy category | |
| Routes of administration | Topical, throat lozenge |
| ATC code | A01AB18 (WHO) D01AC01 (WHO) G01AF02 (WHO) QJ02AB90 (WHO) |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Poor absorption by mouth (lozenge), negligible absorption through intact skin (topical) |
| Protein binding | 90% |
| Metabolism | Liver |
| Biological half-life | 2 hours |
| Identifiers | |
| |
| CAS Number |
23593-75-1 |
| PubChem (CID) | 2812 |
| IUPHAR/BPS | 2330 |
| DrugBank |
DB00257 |
| ChemSpider |
2710 |
| UNII |
G07GZ97H65 |
| KEGG |
D00282 |
| ChEBI |
CHEBI:3764 |
| ChEMBL |
CHEMBL104 |
| ECHA InfoCard | 100.041.589 |
| Chemical and physical data | |
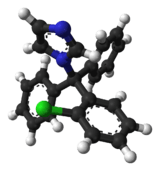
| Formula | C22H17ClN2 |
| Molar mass | 344.837 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| (verify) | |
Clotrimazole, sold under the brand name Canesten among others, is an antifungal medication. It is used to treat vaginal yeast infections, oral thrush, diaper rash, pityriasis versicolor, and types of ringworm including athlete's foot and jock itch. It can be taken by mouth or applied as a cream to the skin or in the vagina.[1]
Common side effects when taken by mouth include nausea and itchiness. When applied to the skin common side effects include redness and burning. In pregnancy, use on the skin or in the vagina is believed to be safe. There is no evidence of harm when used by mouth during pregnancy but this has been less well studied. When used by mouth, greater care should be taken in those with liver problems. It is in the azole class of medications and works by disrupting the cell membrane.[1]
Clotrimazole was discovered in 1969.[2] It is on the World Health Organization's List of Essential Medicines, the most important medications needed in a basic health system.[3] It is available as a generic medication.[1] The wholesale cost in the developing world as of 2014 is 0.20–0.86 USD per 20gm tube of cream.[4] In the United States a course of treatment typically costs less than 25 USD.[5]
Medical uses

It is commonly available without a prescription in various dosage forms, such as a cream, vaginal tablet, or as a prescription troche or throat lozenge (prescription only). Topically, clotrimazole is used for vulvovaginal candidiasis (yeast infection) or yeast infections of the skin. For vulvovaginal candidiasis (yeast infection), clotrimazole tablets and creams are inserted into the vagina. Troche or throat lozenge preparations are used for oropharyngeal candidiasis (oral thrush) or prophylaxis against oral thrush in neutropenic patients.
Clotrimazole is usually used 5 times daily for 14 days for oral thrush, twice daily for 2 to 8 weeks for skin infections, and once daily for 3 or 7 days for vaginal infections.[6]
Clotrimazole is may be compounded with a glucocorticoid, such as betamethasone, in a topical cream for the treatment of tinea corporis (ringworm), tinea cruris (jock itch) and tinea pedis (athlete's foot). Although FDA approved, clotrimazole-betamethasone combination cream is not the preferred treatment for dermatophyte infections due to increased side effects from the topical glucocorticoid. Although temporary relief and partial suppression of symptoms may be observed with the combination therapy, glucocorticoids can elicite an immunosuppressive response and rebound effect that results in more severe infection typically requiring systemic antifungal agents to treat the disease. Combination creams are best avoided in order to improve treatment outcome, reduce the possibility of skin atrophy associated with prolonged topical glucocorticoid use, and to limit the cost of treatment. It can be effective in treating chronic paronychia. The preferred treatment of tinea infections is therefore with clotrimazole monotherapy.[7]
Topical and oral clotrimazole can be used in both adults and children.
Additionally, clotrimazole may be used to treat the sickling of cells (related to sickle cell anemia).[8][9]
Pregnancy
Small amounts of clotrimazole may be absorbed systemically following topical and vaginal administration. However, this may still be used to treat yeast infections in pregnant women.[10]
Side effects
Side effects of the oral formulation include itching, nausea, and vomiting. >10% of patients using the oral formulation may have abnormal liver function tests. Side effects include rash, hives, blisters, burning, itching, peeling, redness, swelling, pain or other signs of skin irritation.[1] For this reason, liver function tests should be monitored periodically when taking the oral clotrimazole (troche). When used to treat vulvovaginal candidiasis (yeast infection), <10% of patient have vulvar or vaginal burning sensation. <1% of patients have the following side effects: Burning or itching of penis of sexual partner; polyuria; vulvar itching, soreness, edema, or discharge [11][12][13]
Clotrimazole creams and suppositories contain oil which may weaken latex condoms and diaphragms.[14]
Drug interactions
There are no known significant drug interactions with topical clotrimazole. However, with oral (troche) clotrimazole, there are multiple interactions as the medication is a CYP450 enzyme inhibitor, primarily CYP3A4. Thus, any medication that is metabolized by the CYP3A4 enzyme will potentially have elevated levels when oral clotrimazole is used. The prescribing physician should be aware of any medication the patient is taking prior to starting oral clotrimazole. Certain medications should not be taken with oral clotrimazole.[15]
Mechanism of action
Clotrimazole works to kill individual Candida or fungal cells by altering the permeability of the fungal cell wall. It binds to phospholipids in the cell membrane and inhibits the biosynthesis of ergosterol and other sterols required for cell membrane production. This leads to the cell's death via loss of intracellular elements.[16][17]
References
- 1 2 3 4 American Society of Health-System Pharmacists (8 February 2016). "Clotrimazole Monograph for Professionals". www.drugs.com. Retrieved 28 October 2016.
- ↑ Walker, S. R. (2012). Trends and Changes in Drug Research and Development. Springer Science & Business Media. p. 109. ISBN 9789400926592.
- ↑ "WHO Model List of EssentialMedicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- ↑ "Clotrimazole". International Drug Price Indicator Guide. Retrieved 28 October 2016.
- ↑ Tarascon Pharmacopoeia 2016 Professional Desk Reference Edition. Jones & Bartlett Publishers. 2016. p. 176. ISBN 9781284095302.
- ↑ "Clotrimazole: MedlinePlus Drug Information". The American Society of Health-System Pharmacists, Inc. Retrieved 17 April 2014.
- ↑ Moriarty, B; Hay, R; Morris-Jones, R (10 July 2012). "The diagnosis and management of tinea.". BMJ (Clinical research ed.). 345: e4380. PMID 22782730.
- ↑ Marieb & Hoehn, (2010). Human Anatomy and Physiology, p. 643. Toronto: Pearson
- ↑ Rodgers, Griffin. "Hydroxyurea and other disease-modifying therapies in sickle cell disease". UpToDate. Retrieved 14 April 2014.
- ↑ "Diseases Characterized by Vaginal Discharge". CDC. Retrieved 17 April 2014.
- ↑ "Clotrimazole: MedlinePlus Drug Information". The American Society of Health-System Pharmacists, Inc. Retrieved 17 April 2014.
- ↑ "Clotrimazole". DrugBank. Retrieved 17 April 2014.
- ↑ "Clotrimazole (Oral)". Lexicomp Online. Retrieved 17 April 2014.
- ↑ "Diseases Characterized by Vaginal Discharge". CDC. Retrieved 17 April 2014.
- ↑ "Clotrimazole". DrugBank. Retrieved 17 April 2014.
- ↑ "Clotrimazole (Oral)". Lexicomp Online. Retrieved 17 April 2014.
- ↑ "Clotrimazole". DrugBank. Retrieved 17 April 2014.